Autonomic dysreflexia (AD) is a potentially life-threatening medical emergency that occurs exclusively in individuals living with a spinal cord injury (SCI) at the T6 level or above. It is a serious condition, and once symptoms develop, prompt intervention is critical. Unfortunately, AD is not always readily recognised outside specialist spinal services, particularly in emergency and pre-hospital settings and urgent improvements are required to enhance patient safety, ensure timely treatment, and potentially save lives
What Is Autonomic Dysreflexia?
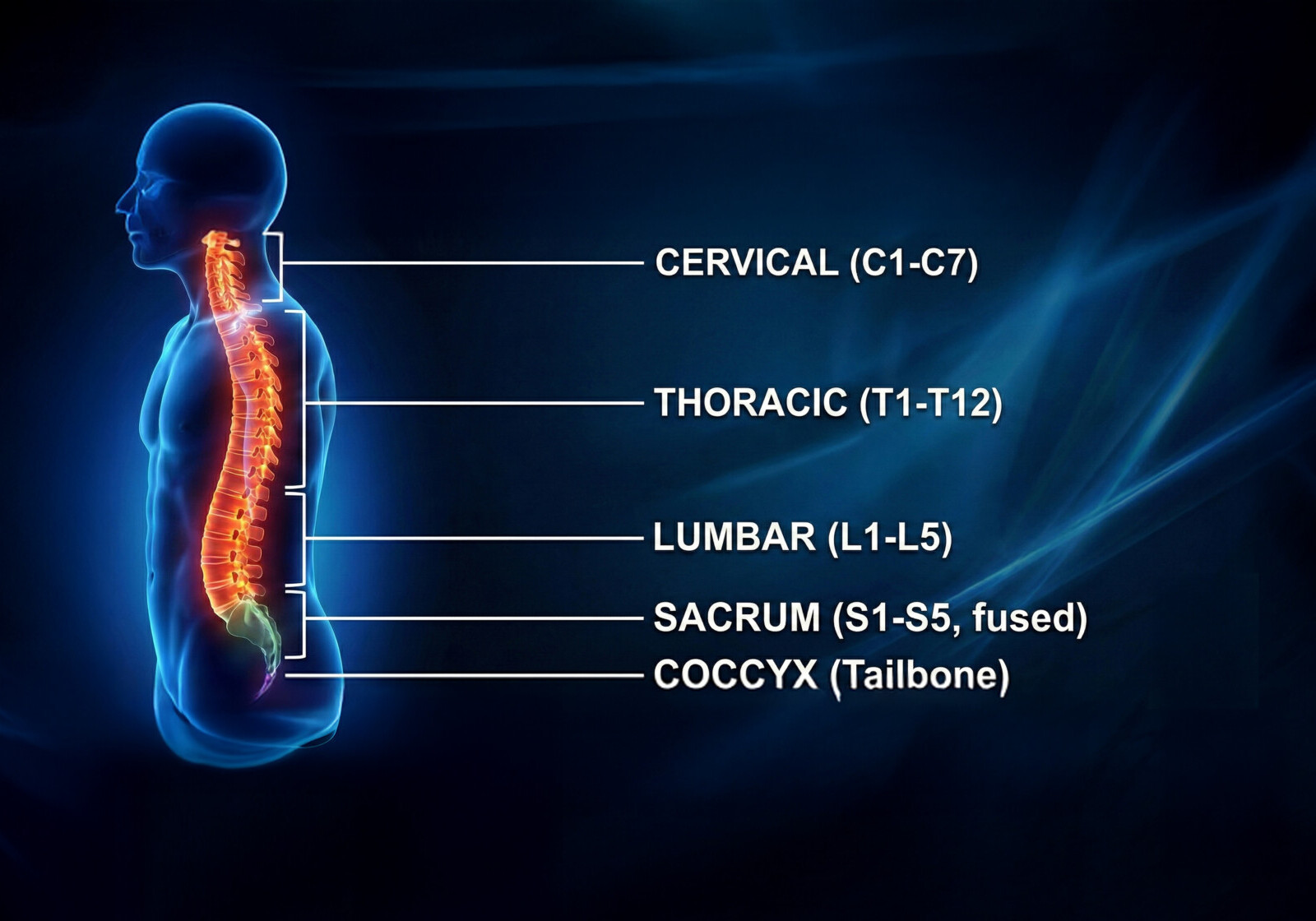
Autonomic dysreflexia is a condition that affects people living with a spinal cord injury at or above the level of the sixth thoracic vertebra (T6) and occurs when a painful or irritating stimulus below the level of injury triggers an uncontrolled response of the autonomic nervous system.
This response causes a sudden and severe rise in blood pressure, which can escalate rapidly and become life-threatening if not treated promptly.
Crucially, the individual may not feel pain in the usual way, making the condition harder to recognise without specific knowledge.
Why Autonomic Dysreflexia Is a Medical Emergency
If untreated, autonomic dysreflexia can lead to:
- Stroke
- Seizures
- Cardiac complications
- Loss of consciousness
- In rare cases, death
Immediate intervention is required. Blood pressure must be checked and the underlying cause identified and relieved as quickly as possible.
Common Signs and Symptoms
In addition to a sudden rise in blood pressure, symptoms of autonomic dysreflexia may include:
- Severe or pounding headache
- Profuse sweating above the level of injury
- Flushed or blotchy skin on the face, neck and upper chest
- Pale, cool skin below the level of injury
- A tight sensation in the chest
- Blurred vision
- Nasal congestion
- Very slow or very fast heart rate
Common Triggers of Autonomic Dysreflexia
Autonomic dysreflexia is triggered by any painful or irritating stimulus below the level of a spinal cord injury such as:
- A distended bladder (e.g. infection, blocked catheter)
- Bowel problem (e.g. constipation, compaction)
- Skin irritation or damage (pressure ulcers, ingrown toenails, burns or scalds)
- Sexual activity
- Menstruation
How Common Is Autonomic Dysreflexia?
While there are currently no published UK national statistics showing how many people present to A&E specifically with autonomic dysreflexia, clinical research provides clear evidence of how common the condition is within the spinal cord injury population.
- Studies suggest that 20–70% of people with SCI at or above T6 will experience autonomic dysreflexia.
- In people with cervical or high thoracic injuries, prevalence rates rise to as high as 90%.
- Some individuals experience recurrent or ‘silent’ episodes, where blood pressure rises dangerously without obvious symptoms, sometimes multiple times a day.
In the UK, it is estimated that over 105,000 people are living with spinal cord injury, with approximately 4,400 to 4,700 new cases occurring each year, AD represents a significant and urgent public health concern, which needs greater awareness, timely recognition, and effective management across all healthcare settings.
Why There Are No Clear A&E Statistics
The lack of UK-wide emergency department data on autonomic dysreflexia highlights an important issue in itself.
The limited data is likely due to:
- Coding limitations, where AD is recorded under broader categories such as spinal cord injury complications or hypertension
- Limited recognition, particularly in non-specialist settings
- Infrequent exposure to AD among emergency clinicians, paramedics and call handlers
- No national registry for SCI complications such as autonomic dysreflexia
As a result, episodes may be treated without being formally documented as AD, making the true scale of the issue difficult to accurately monitor.
The Importance of Emergency Recognition and Triage
For individuals at risk of autonomic dysreflexia (AD), rapid response is crucial. However, there is increasing concern that AD is not consistently recognised as an immediate emergency by call handlers, ambulance services, or A&E departments. In some instances, calls may be assigned a lower priority, resulting in delays to treatment.
Consequently, organisations such as the Spinal Injuries Association have emphasised the need for better awareness and have recommended that autonomic dysreflexia be formally classified as a Category 1 emergency, reflecting the potentially life-threatening nature of the condition.
What People with SCI and Their Support Networks Can Do
People at risk of autonomic dysreflexia are encouraged to:
- Carry an AD emergency card or care plan
- Clearly state “autonomic dysreflexia” when calling 999
- Ask for blood pressure to be checked immediately
- Ensure family members, carers and support staff understand the signs and urgency
Spinal Cord Injury Rehabilitation
STEPS Rehabilitation® delivers specialist spinal cord injury rehabilitation services in a purpose-built residential facility. Explore our Spinal Cord Injury Rehabilitation page to learn more about our programmes.
Sources
- Spinal Injuries Association – Autonomic Dysreflexia guidance
- Autonomic Dysreflexia - StatPearls - NCBI Bookshelf
- Paramedic Practice Journal: Pre-hospital treatment of autonomic dysreflexia
- MSD Manuals (UK): Autonomic Dysreflexia of the Spinal Cord
- Christopher & Dana Reeve Foundation – Autonomic Dysreflexia resources