Balance is the ability to maintain the body’s centre of mass over its base of support.
(Shumway cook, 2007)
“An even distribution of weight enabling someone or something to remain upright and steady or allows you to move without falling over or recover from a trip.”
Balance is achieved and maintained by utilising a complex set of sensorimotor control systems as well as muscle strength and flexibility. These systems are highly integrated and interconnected networks within the nervous system, allowing people to perceive their environment, make decisions based on sensory input, and execute precise and coordinated movements. A functioning balance system enables us to make automatic postural adjustments in response to external input such as visual input, gravity, speed of movement and direction. These systems include:
- Sensory systems, including vision, proprioception, auditory, vestibular, and tactile feedback.
- Central Nervous System
- Motor systems
- Cerebellum
- Basal Ganglia
- Spinal reflexes
Balance is often taken for granted as it is something that develops from birth and is a part of progression through childhood milestones. We learn from an early age how to walk on a variety of surfaces without tripping, to step up/down and over obstructions, change direction quickly, maneuver in the dark without falling. For those who suffer with an impairment in any of the above systems, balance can become challenging and fatiguing.
Some medical conditions which could affect these systems are:
- Disorders of the central nervous system e.g.: multiple sclerosis, Parkinson's disease, stroke
- Vestibular issues e.g.: Meniere's disease, BBPV and PPPD which can cause dizziness and vertigo.
- Conditions which distort vision e.g.: Cataracts, macular degeneration, and glaucoma
- Muscle weakness/imbalance (following injury, disease, or medication)
- Nerve damage (through injury or disease)
At STEPS, due to the complexities of our clients, it is seldom a single component that affects their balance and is more often a combination of factors that need to be explored and treated to address an individual's balance needs.
What we do at STEPS:
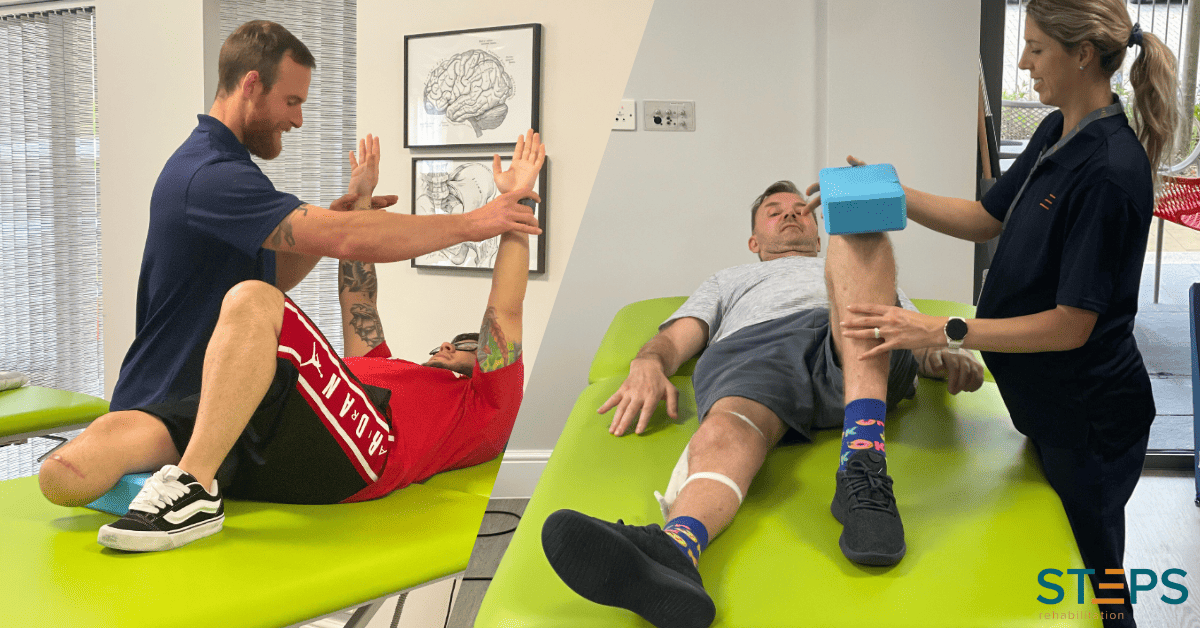
We work as an Interdisciplinary team to ensure that all the factors contributing to an individual's balance issues are addressed; this involves:
- Medication review with consultant
- Indicated assessments, e.g.: Vestibular, sensory, muscle strength, coordination.
- Formulation of identified needs
Once the contributing factors are established an individualised program is developed. Programmes typically include a combination of the following:
Traditional land-based therapy:
- Muscle strengthening and stretching programmes.
- Vestibular rehabilitation, head and neck range of motion (ROM), head and eye dissociation, (Cawthorne- Cooksey exercises)
- Vestibular treatment eg: Epleys, This is a simple treatment that involves you turning your head in a series of movements. The movements are specifically designed to use gravity to dislodge the crystals from the semi-circular canals and return them to where they belong, treating the symptoms of vertigo or for Benign paroxysmal positional vertigo (BPPV) is a problem in the inner ear. It is the most common cause of vertigo, which is a false sensation of spinning or movement.
- Joint sessions: Physiotherapist /Neurologic Music Therapist (NMT) focus on gait re-education using Rhythmic Auditory Stimulation technique, which is a is a scientific walking technique that uses a metronome rhythm and musical cues to entrain walking pattern and acts as a facilitating stimulus for training efficient movement patterns and optimum gait.
Our Groups:
- Balance group: This is run jointly by a Senior Physiotherapist (PT) and Neurologic Music Therapist (NMT). The balance group works with a variety of Neurologic Music Therapy techniques and Physiotherapy interventions. Rhythm alongside musical cues and simple verbal cues, prompts specific movement patterns designed and led by the physiotherapist. The aim of these exercises are to promote rehabilitation of postural control, balance, weight shifting stability, re-orientation of one’s centre of gravity, proprioception, coordinated arm movements and efficient gait.
- Circuit group: This is run by Therapy Assistants. The content of the group is designed to promote cardiovascular fitness, muscle strength, proprioception, and coordination in a fun environment. The way the group is designed allows for people with a variety of conditions, working at different levels to attend and benefit.
- Pilates: This is run by our Specialist Physiotherapists for clients of varying levels and abilities. It focuses on core activation/awareness, proprioception, and coordination alongside strengthening and stabilization which all play a part in reducing the risk of falls.
- Community trips: These are planned and run by the Occupational therapy, nursing and physiotherapy teams to ensure that skills are transferrable to the community and not just within STEPS. These trips can also challenge clients, giving more information about what further issues may need addressing. The trips are planned with clients to ensure to be as valuable as possible both physically and psychologically. They allow outdoor mobility practice with distraction, requiring higher level balance with cognitive challenges.
Aquatic Therapy:
The properties of water facilitate a variety of ways of challenging the balance systems.
- Hydrostatic pressure (increasing sensory feedback)
- Turbulence and Drag (can aid strengthening and challenge balance)
- Buoyancy (The centre of buoyancy along with the centre of gravity allows the practice of Metacentre work which challenges proprioception, strength, stabilisation, and correction)
Technology:
- Mindmotion GO: Integrated game play utilising augmented reality and tracking technology to challenge identified deficits.
- Mindpod and Arm-Motus: Different modalities that utilise game play for the upper limb, which can be completed in a variety of postural sets, in order to challenge the appropriately identified systems.
- Physio Sense-Balance mat: Allows for assessment of weight distribution as well as providing visual feedback.
- Virtual Reality (VR): Can reduce symptoms such as vertigo, dizziness, and tolerance to visual motion, Improve gaze stabilization and postural stability.
Why we do this?
- To promote Neuroplasticity and learning – by incorporating balance training consistently throughout a rehabilitation programme, it allows the repetition to encourage neural networks in the brain to change through growth and reorganisation.
- Strengthening principles - overload, progression, and specificity.
- Righting reactions/ balance reactions – APAS and CPAS (anticipatory postural adjustment and compensatory postural adjustments)- aim to maintain balance through maintaining equilibrium.
- Vestibular theories - Vestibular rehabilitation therapy (VRT) is an exercise-based treatment program designed to promote vestibular adaptation and substitution. The goals of VRT are 1) to enhance gaze stability, 2) to enhance postural stability, 3) to improve vertigo, and 4) to improve activities of daily living.
- NMT theories – muscle co-ordination, balance and strength, memory recall and develops essential motor skills. “The strong rhythmic pulse and structure of music provide the preparation, activation, and re-activation of specific and targeted movement patterns.
The complexity of the balance system can make diagnosing and treating balance issues challenging. It is essential to understand the underlying cause; work with and educate the client to provide an individualised treatment in which they will engage.